U.S. researchers say they've been able to modify a patient's immune system T cells, turning them into “serial killer” cells which zero in on cancer and obliterate it.
It’s being called a breakthrough in the treatment of a form of leukemia, a hard to treat and usually fatal blood cancer.
Chronic lymphocytic leukemia (CLL) is marked by a slow increase in immune system white blood cells, called B lymphocytes. These B cells, as they're known, are manufactured by the bone marrow, the spongy tissue inside bones that also manufactures red blood cells.
Eventually, the healthy blood cells are crowded out by the proliferating B cells, the patient experiences bone marrow failure, and - without a bone marrow transplant - dies.
A transplant of healthy bone marrow from a donor has been the only treatment and potential cure for chronic lymphocytic leukemia. But it is very difficult to find a match and many people with CLL die while waiting. Even with a transplant, experts say only about half of CLL patients survive the procedure.
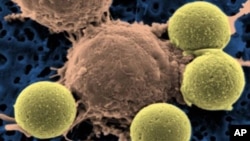
Three CLL patients who had run out of treatment options were selected for an experiment at the University of Pennsylvania. Researchers genetically engineered another one of their immune system cells, the T lymphocytes, to attack cancerous B cells.
Carl June, a professor of pathology and laboratory medicine at the school’s Abramson Cancer Center, was the study’s lead author.
“The actual trial exceeded our wildest outcome and imagination actually," says Carl June, professor of pathology and laboratory medicine, who was the study’s lead author, "because what we found is all three patients have had a remarkable anti-tumor response and that literally pounds of leukemia have been eradicated in all three patients.”
Two of the three CLL patients had a complete remission of their disease and there was a significant improvement in the third.
Watch related video story by Vidushi Sinha
The T cells were genetically modified using a harmless virus, which carried an anti-body called a chimeric antigen receptor (CAR). Antibodies are immune system proteins which are produced in response to an infection.
The CAR was engineered to bind to another protein called CD19 that’s present on the surface of normal B lymphocytes and all CLL tumor cells.
Scientists say the modified T cells, injected into the patients following standard chemotherapy, homed in on the cancerous B cells inside the bone marrow, each T lymphocyte killing thousands of tumor cells.
Researcher Michael Kalos says the team also engineered a signaling molecule that binds to CD19, triggering the continued production of thousands of T cells. The genetically engineered cells act as sentries against cancerous B cells should they return.
“We saw a substantial number of cells remaining circulating and in the marrow of patients very, very late after infusion, nine to 12 months, entirely unprecedented in the field," says Kalos. "And finally we saw that those cells, not only did they remain there, but they were able to be triggered, recognize and kill cancer cells when they encountered them again.”
In a report describing the so-called “serial killer” T cell therapy in the New England Journal of Medicine, researchers say it completely obliterated cancer cells in a 64-year-old man with CLL three weeks after treatment, and three to six months later, researchers could detect no sign of disease.
The patient’s marrow began manufacturing healthy B cells to replace the ones that were destroyed as "collateral damage" by the therapy. Cells that did not express CD19 were unaffected.