Women who have Type 1 diabetes, a condition in which the body does not produce the hormone insulin, might someday be successfully treated with a transplant of insulin-producing cells grown from cells in their uterus.
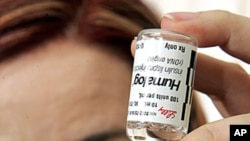
Researchers at Yale University in New Haven, Connecticut, took the stem cells from the human endometrium, or lining of the uterus, and converted them into insulin-producing islet or beta cells. Stem cells are master cells that, given the right nutrients and growth factors, can be coaxed to grow into any type of cell in the body. Normally, endometrial stem cells generate the lining inside the womb that is shed each month during menstruation.
After converting the endometrial cells into islet cells, scientists injected them into the membrane surrounding the kidneys of diabetic mice whose pancreases produced no insulin, a hormone used by mammals to convert glucose from food into energy.
Louis DePaolo is head of the Reproductive Sciences Branch at the U.S. National Institute of Child Health and Human Development, which funded the research. DePaolo says the animals that received the islet cell transplant were more alert and healthier-looking than the untreated mice, which developed cataracts and dull fur.
But DePaolo says the transplant did not cure the treated mice of their diabetes. They still suffered from high blood sugar, an indication that not enough insulin was being produced to control the disease.
"You are talking about at least 20- or 30-fold less secretion of insulin by these cells than cells that you are actually taking from the pancreas; not ones that have actually been converted to pancreatic cells," DePaolo noted.
For that reason, DePaolo says it's likely to be many years before stem therapy is used to treat diabetes in humans. For one thing, he says scientists need to figure out how to get the newly-created beta cells to produce more insulin.
The findings in the latest study would be of most benefit to individuals suffering from Type 1 diabetes, in which the pancreas does not produce enough insulin, causing abnormally high or low levels of sugar in the blood. The treatment would be less helpful for the more common Type 2 diabetes, in which the pancreas produces insulin, but the body has difficulty using it.
The mice in the Yale experiments were bred to lack an immune system so they did not reject the transplanted human beta cells. DePaolo says in humans, diabetic women whose bodies do not produce insulin could potentially have beta cells tailor-made from their own endometrial stem cells.
"So that [way] you wouldn't have the immune response," DePaolo noted. "And that's one of the highlights of this study, is that the cells that are obtained are readily available from the uterus from women who undergo hysterectomy, for one reason or another they can obtain these stem cells."
Using the same laboratory techniques, Yale researchers also converted endometrial stem cells into healthy brain cells that, theoretically, could be used to replace the cells that go awry in Parkinson's disease. The procedure has not been tested yet in animals.
The study on converting endometrial cells into insulin-producing islet cells is published in the journal Molecular Therapy.
Reproductive Cells May Some Day Treat Women with Diabetes