Food is medicine. That’s what dozens of low-income patients in the Washington area discover through DC Greens' Fruit and Vegetable Prescription Program.
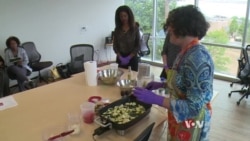
When they visit one of the four participating health care centers, they receive more than medical checkups. They get nutrition information, participate in cooking lessons and do some exercising.
And they‘re given prescriptions — not for medication, but for free produce.
The weekly program provides patients with what they usually cannot afford, to improve their diet and their health.
Food education
DC Greens, a food education and policy group, has been running the program for four years in conjunction with Unity Health Care Clinics.
Lauren Shweder Beil, executive director of DC Greens, said that over that time, they have served close to 1,000 patients and their families.
The patients learn about the nutritional value of the different fruits and vegetables available each season, and why they should eat more fresh produce instead of processed and canned foods. And they have a chance to spend time talking to health care providers.
“We’ve gotten feedback from the doctors saying, 'You know, this program lets me treat patients the way I always have wanted to. It’s one thing to say, "Go out and buy healthy food," and it’s another thing to be able to give them a way to follow my medical advice.' ”
Nurse practitioner Sorelle Cooper, assistant medical director at Unity Health Care, agrees.
“When we see them," she said, "we have 15 minutes in a visit to talk to them, and it’s really difficult to find time within that short period to really get into depth discussion about how to change their eating, how to change their behavior so that they can be healthier people.”
'Food desert'
By spending some quality time with the patients outside the exam room, health care providers are able to engage them in discussions about ways to change their lifestyles.
“Our patients live in an area that’s considered a ‘food desert,’ where having access to fresh fruits and vegetables is limited," Cooper said. "We know that those sorts of foods can do things like help reduce inflammation. Health problems like diabetes, hypertension, obesity [and] some cancers have been linked to diet. So having patients understand how to improve their diet overall with ingredients naturally grown, things that are not processed, has a huge impact on their long-term health.”
Cooper said the results have been positive and encouraging.
“We’ve seen great weight loss," she said. "We’ve seen patients get serious control of their diabetic status, and literacy has gone up.”
The Fruit and Vegetable Prescription Program, trademarked by Wholesome Wave, has made a difference for patient Joyce Pratt.
“The program has really been educating for me," she said. "I’ve been diabetic for about 10 years. I’m on insulin. I had no idea of the proper way that I’m supposed to eat.”
Every week, participants get their prescriptions for fresh produce, and they fill them, for free, at a mobile farmers market that pulls up at the clinic.
Patients like Teresa Farmer say they have been inspired to eat more fruits and vegetables. More important, they are sharing what they’ve learned with their families.
“My daughter is pre-diabetic, and everything I cook, I have her taste it,” Farmer said.
The weekly visits to the clinic end with some physical activity, such as a brisk walk around the block — all part of a prescription for a positive lifestyle change.