As options for cancer patients become increasingly complicated, and expensive, the most influential source for U.S. oncology treatment guidelines will for the first time offer a tool to assess the costs versus benefits of available therapies.
The National Comprehensive Cancer Network (NCCN) says its new tool will provide a clearer picture of the relative value of medication options, particularly in cases where a very expensive therapy does little to improve survival.
Doctors developing the measures expect them to shift demand away from less effective treatments, influencing the prices drugmakers are able to charge. They say they are responding to the needs of patients who are having to pay much more for their own care, with higher health insurance premiums, co-payments and deductibles, and want to know the value of their treatments.
The NCCN, an alliance of 26 cancer centers, envisions the new tool as a supplement to its widely followed guidelines for oncology care, which set out protocols for treating a range of cancers based on diagnosis, disease stage and other factors, such as age.
Other medical groups are also trying to address the cost issue, but not as directly as the NCCN. The American Society of Clinical Oncology (ASCO) is developing its own tool for valuing treatments, but says that its "net health benefit" scores will not consider costs, although prices will be noted alongside the scores.
In June, New York's Memorial Sloan Kettering Cancer Center launched an interactive calculator, called "DrugAbacus," that allows users to decide how much one of 54 newer drugs should cost based on factors like side effects and novelty.
The NCCN scale, to be launched in mid-October, will employ "evidence blocks" that assign a score of up to five points for each of five measures - price, effectiveness, safety, quality and consistency of clinical data. Initially, it will evaluate drugs used for multiple myeloma and chronic myeloid leukemia.
Similar guidelines are expected for most other types of cancer by the end of 2016.
"A company that has an effective drug that's appropriately priced should welcome these blocks," said Dr. Robert Carlson, NCCN's chief executive. If a drug is overpriced, "that's very important information for everybody."
Currently, prescribing patterns can be inconsistent, determined by an individual physician's understanding of published data about a drug, patient preferences and habit.
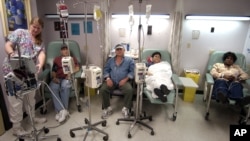
U.S. oncologists also can make a profit on intravenous drugs
administered in their offices - calculated as a percentage of a drug's cost - creating a possible financial incentive for choosing higher-priced therapies.
The NCCN says the assessment of each medication will be presented in a simple, tabular form - with each of the five components colored in to represent a score of one to five. The information will appear on its website and in printed literature.
Eventually, the comparison tool will be incorporated into healthcare technology systems used by hospitals, including products from IBM Watson and McKesson.
Threat to drugmakers
The sort of cost-benefit analysis NCCN has undertaken could threaten drugmakers like Roche Holding AG, Novartis AG and Celgene Corp, which earn billions of dollars annually from cancer therapies that may do little to extend a patient's life or come with severe side effects.
Worldwide spending on cancer medications reached $100 billion in 2014, up from $75 billion just five years earlier, according to IMS Health. U.S. spending accounted for 42 percent of the total.
Drugmakers are already concerned about the accuracy of the information NCCN plans to present and worried that health insurers will seize on the new guidelines to drop coverage of some drugs, said Randy Burkholder, vice president of policy and research at the Pharmaceutical Research and Manufacturers of America.
The trade group does not have full details of the NCCN's plans, and will comment on the guidelines once they are public, he said.
The NCCN website has some 700,000 registered users, and more than 6 million copies of its guidelines were downloaded last year.
The two largest U.S. payers of health costs - UnitedHealth Group and the federal government's Medicare plan for seniors - rely on NCCN guidelines to shape their oncology reimbursement policies.
"Many, if not most, of the others use our guidelines either directly or indirectly," Dr Carlson said. The current guidelines don't analyze costs, though, and top oncologists have questioned whether some treatments are worth the price.
For example, Roche's Avastin offers lung cancer patients an additional 1.5 to 2 months before their disease worsens, "but that changes the cost per month of treatment from something in the hundreds of dollars, to close to $10,000," said Dr. Lowell Schnipper, chief of hematology/oncology at Beth Israel Deaconess Medical Center in Boston. He chairs the ASCO task force studying the value of cancer care.
A recent study showed Stivarga, sold by Bayer AG, added about two weeks of "quality adjusted" life, at a median price of nearly $40,000, for previously treated patients with advanced colorectal cancer.
The researchers said the drug, which causes side effects including swelling of the hands and feet, has become the standard of care for that indication since entering the U.S. market in 2012.
Patient advocates have traditionally warned against treatment decisions that factor in a drug's price, saying such considerations could lead to "rationed" healthcare. But at the same time, patients worry about costs.
A recent poll by the Kaiser Family Foundation found than 87 percent of Americans surveyed want changes to U.S. law that would allow Medicare to negotiate drug discounts.
Dr. Derek Raghavan, president of Levine Cancer Institute at Carolinas HealthCare System, says doctors need much more real-world information at their disposal, including a cost-benefit analysis of side effects.
"If Drug B costs 70 percent of Drug A, but has a side effect profile that brings every second patient to the hospital for a four-day admission, then it does not have value," he said.