Researchers have developed the first non-invasive method of detecting malaria infection using a laser beam scanner. The painless test appears to be 100 percent accurate and does not require using any blood.
Currently, the gold standard of malaria testing is examining a blood smear under the microscope for evidence of the deadly parasite. A diagnosis requires trained technicians, expensive equipment and time, things that are not always available in poorer and more remote parts of the world.
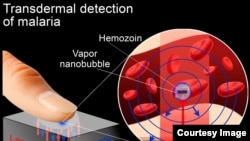
But so-called “vapor nanobubble” technology would eliminate the need to draw any blood. It only requires an individual to place a finger on a laser device, according to Dmitri Lopotko, a researcher with the department of biochemistry and cell biology at Rice University in Houston, Texas.
“We shine a very short light pulse through the skin. And this light pulse is absorbed only by malaria parasites because of the wavelength we use. And in response to this short light pulse, the parasite literally explodes,” he said.
The light pulse - from a low-powered laser - is trained on an extremely tiny particle called hemozoin that is produced by the malaria parasite once it has infected red blood cells. Lopotko said hemozoin crystals are not found in normal red cells.
As they are heated by the laser, the crystals create a tiny vapor of miniscule bubbles inside infected cells.
When the bubbles burst, Lopotko said they have a unique acoustic signature, which scientists can hear and count.
“You can detect just a few infected cells in a million normal cells,” he said.
Lopotko said there were no false positive results in experiments with the device, making the nanobubble technology extremely accurate even in the earliest stages of a malaria infection when treatment is extremely important.
The portable battery-powered device won’t be cheap, however, costing around $10,000-$20,000 each to manufacture.
“But each device will be capable to screen more than 200,000 people per year. So the cost of analysis for each patient will be less than 50 cents,” he said.
And it can be used by non-medical personnel to diagnose suspected cases of malaria.
Lopotko said the light beam used by this rapid, non-invasive technology is less powerful than the familiar laser pointer and has been shown to be safe in volunteers. The next step is clinical trials at a hospital in Houston that cares for patients infected with malaria, followed shortly thereafter by global clinical trials in 2014.
An article describing the transdermal malaria detection device is published in the journal Proceedings of the National Academy of Sciences.
Currently, the gold standard of malaria testing is examining a blood smear under the microscope for evidence of the deadly parasite. A diagnosis requires trained technicians, expensive equipment and time, things that are not always available in poorer and more remote parts of the world.
But so-called “vapor nanobubble” technology would eliminate the need to draw any blood. It only requires an individual to place a finger on a laser device, according to Dmitri Lopotko, a researcher with the department of biochemistry and cell biology at Rice University in Houston, Texas.
“We shine a very short light pulse through the skin. And this light pulse is absorbed only by malaria parasites because of the wavelength we use. And in response to this short light pulse, the parasite literally explodes,” he said.
The light pulse - from a low-powered laser - is trained on an extremely tiny particle called hemozoin that is produced by the malaria parasite once it has infected red blood cells. Lopotko said hemozoin crystals are not found in normal red cells.
As they are heated by the laser, the crystals create a tiny vapor of miniscule bubbles inside infected cells.
When the bubbles burst, Lopotko said they have a unique acoustic signature, which scientists can hear and count.
“You can detect just a few infected cells in a million normal cells,” he said.
Lopotko said there were no false positive results in experiments with the device, making the nanobubble technology extremely accurate even in the earliest stages of a malaria infection when treatment is extremely important.
The portable battery-powered device won’t be cheap, however, costing around $10,000-$20,000 each to manufacture.
“But each device will be capable to screen more than 200,000 people per year. So the cost of analysis for each patient will be less than 50 cents,” he said.
And it can be used by non-medical personnel to diagnose suspected cases of malaria.
Lopotko said the light beam used by this rapid, non-invasive technology is less powerful than the familiar laser pointer and has been shown to be safe in volunteers. The next step is clinical trials at a hospital in Houston that cares for patients infected with malaria, followed shortly thereafter by global clinical trials in 2014.
An article describing the transdermal malaria detection device is published in the journal Proceedings of the National Academy of Sciences.